What is Peripheral Arterial Disease?
Peripheral arterial disease (PAD) is a condition in which plaque buildup in the walls of blood vessels causes them narrowing or blockage, contributing to a variety of uncomfortable symptoms such as sores and ulcers that won’t heal on their own, burning sensations in the feet, and numbness or tingling in the extremities. If left untreated, severe peripheral arterial disease may lead to critical limb ischemia, a condition where blood flow is drastically decreased to the lower extremities, significantly increasing a patient’s risk of amputation. Patients who are experiencing symptoms of Peripheral arterial disease (PAD) are encouraged to set up a consultation with a StrideCare vein specialist.
What is Peripheral Arterial Disease?


What Causes PAD?

What Causes PAD?
Common risk factors that contribute to the onset of this condition include diabetes, obesity, sedentary lifestyle, smoking, high blood pressure, genetics, and a history of high cholesterol.
What are the Symptoms of PAD?

Coldness in the lower leg or foot

No pulse or weak pulse in legs and feet

Shiny skin on legs

Leg numbness or weakness

Sores on the toes, feet or legs that won’t heal
What Treatments are Available for PAD?
There are Many Treatments for PAD Available at StrideCare Including:
Diagnostic Arterial Ultrasound
A non-invasive test that uses ultrasound technology to get a full view of the circulatory system.
Angiography
Angioplasty
A minimally invasive treatment that uses advanced laser technology to clear plaque on large blood vessels.
StrideCare
Patient Reviews


4.89 Average Online Review Score











StrideCare Leverages athenaOne to Enhance Financial and Operational Results, Improve Clinical Workflows
2 Min Read CASE STUDY: Transitioning all practices onto one united system gives StrideCare invaluable access to data

When are Varicose Veins More than Just a Cosmetic Concern?
2 Min Read Learn about varicose veins, prevention tips, and treatment options from StrideCare’s vein specialists in Texas.
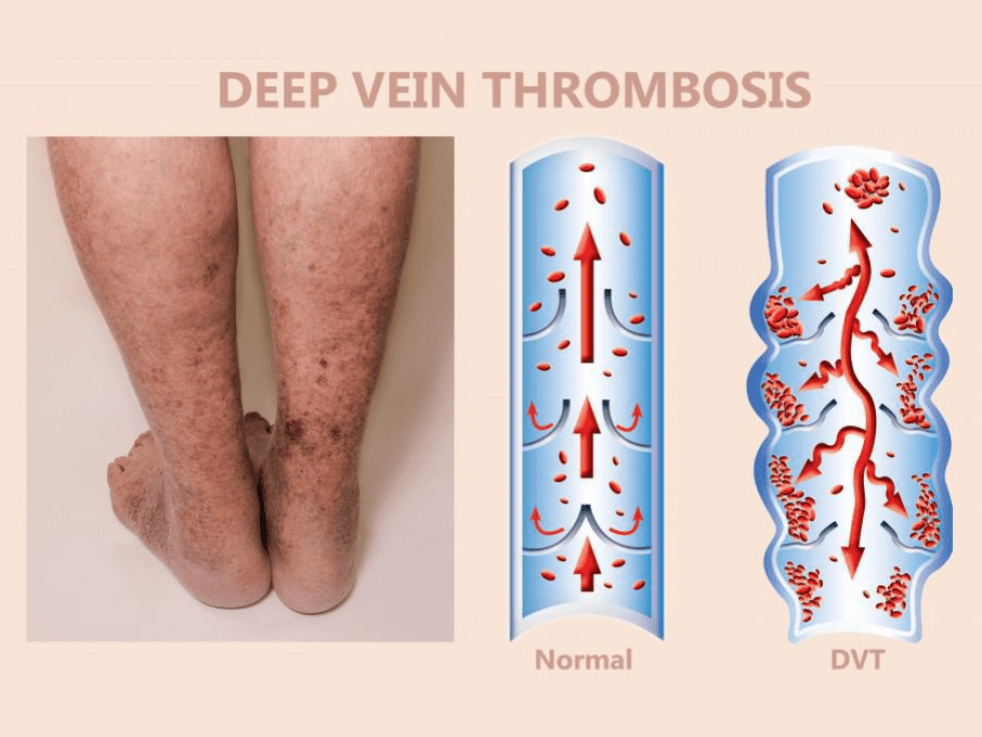
Puffy Legs are One of the First Signs of Deep Vein Thrombosis
3 Min Read Learn the symptoms of deep vein thrombosis (DVT) and seek immediate evaluation at StrideCare for expert care and treatment.


